MALE INFERTILITY
MALE INFERTILITY TREATMENT IN FOLLOWING CASES
- Oligospermia -low number of sperm
- Azoospermia- no sperms present
- Asthenospermia-slow moving sperms
- Oligoasthenospermia-low sperm count with sluggish sperms
- Hematospermia (blood in the semen)
- Anejaculation (no semen after intercourse)
Perhaps because the woman carries the baby, we often consider infertility solely a female problem. In fact, up to 50 percent of all infertility cases involve the male partner. If male fertility issues are suspected based on the results of a semen analysis, he is refered to a male fertility specialist or an andrologist, who specializes in male reproductive problems. Just as reproductive endocrinologists are gynecologists sub-specialized in treating female infertility, andrologists are urologists specially trained to treat male infertility.
As with female infertility, there are a number of treatments to successfully address various male infertility diagnoses. When recommending a given male fertility treatment option, we consider three important factors:
- Cause of infertility, if identifiable
- Severity of the sperm abnormality
- Age of the female partner
The male fertility evaluation will include a sperm count, and usually a panel of hormone blood tests, a physical and urogenital examination, and possibly genetic tests and/or sperm function testing.
Semen Evaluation
Most men will initially be diagnosed with a potential male factor problem based on the results of an ejaculated sperm specimen.
Semen Analysis-WHO Minimal Standards of Adequacy
- Ejaculate volume----------1.5-5.0cc (milliliters)
- Sperm Concentration----->20 million sperm per cc
- Motility--------------------->50%
- Forward Progression------2 (scale 1-4)
- Morphology----------------30% normal forms (WHO criteria)
- Morphology---------------->4% normal forms (Krueger criteria)

Total Motile Count
Sometimes only one sperm parameter is abnormal and sometimes several are abnormal. An indicator useful in determining overall fertility is called the total motile count. This number represents the total number of motile sperm in the ejaculate. The total motile count is calculated thus:
Ejaculate volume X Sperm Concentration X %Motility = TMC
If the TMC is 20 million sperm or less, there is likely to be a 'significant' male factor problem. Men with a TMC consistently less than 5 million are said to have 'severe' male factor infertility.
Morphology
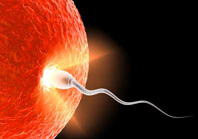
Another important parameter in the semen analysis is the morphology, or shape of the sperm. The shape of the sperm is a reflection of proper sperm development in the testicle, or spermatogenesis. Men with a defect in sperm maturation tend to have problems with sperm morphology and may then be at risk for failure of their sperm to fertilize their partner's eggs.
